
Sugar is the new Crack.
We’ve been told that SUGAR causes cavities and sugar replacements are “healthy”.
We were lied to.
Sugar DOES NOT cause cavities (directly), but it can lead to tooth decay.
ACID is what actually causes cavities. And bacteria in the oral cavity can produce these acids as a byproduct of sugar. In fact, in the absence of these sugar-loving bacteria, Strep Mutans and Lactobacillus species, decay is unlikely.
Unlikely, but not impossible. There are other sources of acid like stomach acid and foods that can, even without bacteria or sugar, cause cavities.
One thing we know for sure is that sugar consumption facilitates the growth of the very bacteria that can use it to produce acid and hence, cavities!
Sugar consumption iis a huge problem for human beings.
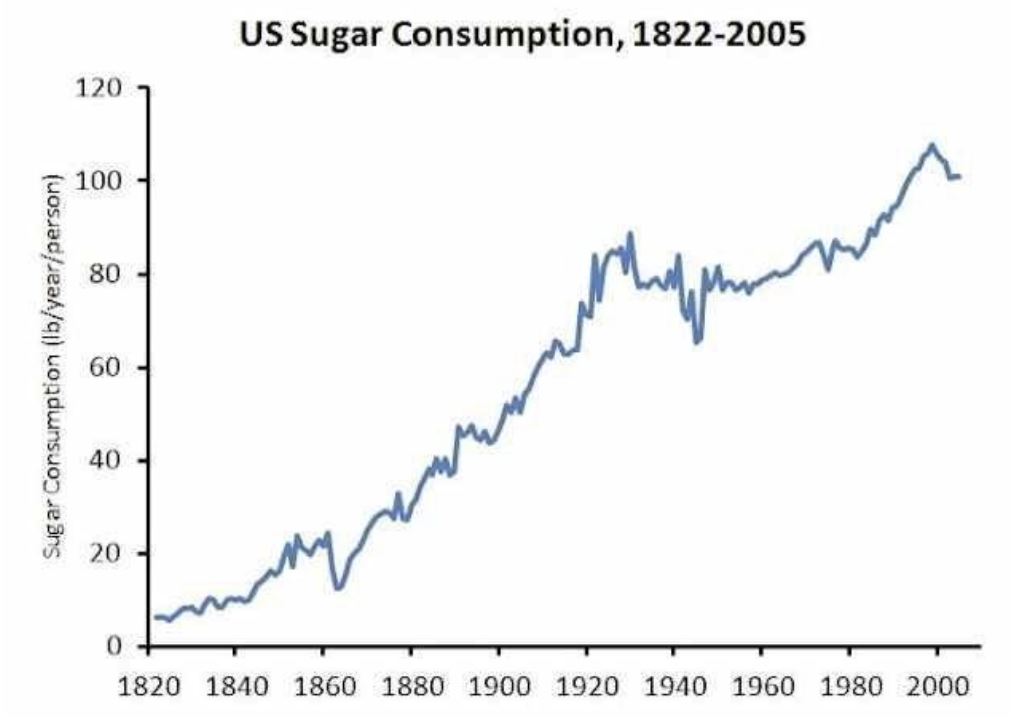
If you were told that, on average, Americans consume over 22 teaspoons of sugar a day, would you be surprised? Well it’s true.
Yes, that was published in a 2005 study. It’s even higher today, over 100 lbs of sugar per person per year in the US.
From 1970 to 2005, sugar in the American diet increased 19%, directly impacting the epidemics of obesity, diabetes and tooth decay. Between 1988 and 2012 the prevalence of Type 2 diabetes rose a whopping 25% in both obese and normal weight populations.
Sugar stimulates the pleasure receptors of the brain much like crack cocaine and heroin does.
In fact, a study by Ahmed, Guillem and Vandalee, published in 2013 showed that on a neurobiological level, sugar is actually more powerful (robust) than cocaine and is even more rewarding and attractive.
Cocaine addicted rats were willing to forgo their fix of cocaine in favor of Oreos! YUM. That’s just how addictive sugar is.
Diabetes and obesity are major contributors to the USA’s $3.2 Trillion expenditure on healthcare in 2015. That’s nearly $10,000 per person, per year and 18% of our GDP. Compare that to the next highest industrialized country, France, which is at 11% and the U.K. at 8.8%.
Hmmm, could our addiction to sugar be the cause?
YES.
Refined, processed carbohydrates are not only easier for us to process; they’re easier for the bacteria in your mouth to process too. Processed foods are built to stay on store’s shelves and ship. Unprocessed foods are more perishable but that’s the way nature intended us to eat. It’s the “paleo” way.
The bacteria in our mouth process the carbohydrates, produce acid and the result is decay. Plus, sugars and refined carbs actually change the makeup of the bacteria in the mouth, what is called the Microbiome.
It’s a combination of the Microbiome of your mouth, the acid coming into your mouth from either food or from your stomach (heartburn or reflux), the hardness of your teeth and the quantity and makeup of your saliva that factors into whether you’ll get decay.
There’s a possible solution to a dry mouth, a bad Microbiome and a sweet tooth. XYLITOL.
This natural, alcohol sugar changes the bacteria in the mouth, promoting safe bacteria and discouraging harmful ones from congregating. Plus, used in gum or sucking candies, Xylitol promotes saliva flow, which also helps reduce decay, remineralizing teeth and even fights gum disease. It also has a higher glycemic index than regular sugars.
Xylitol has been approved by the U.S.’s FDA, the World Health Organization and the European Union’s Scientific Committee for Food.
One caveat. Like chocolate, Xylitol is dangerous for dogs, so keep the stuff away from Fido.
Funny enough, Theobromine, which is included in Linamel Toothpaste, is an extract from chocolate.
So cut down on the sugars, not only are they bad for your overall health including causing obesity, diabetes, heart disease and other maladies, but sugar also leads to tooth decay, which means more frequent trips to your dentist!

If you neglect to look after your teeth, then you’re also neglecting the health of your entire mouth. Doing so is a sure-fire way to lead yourself into pain and discomfort, bleeding gums, bad breath, and gum disease. Your mouth is teeming with bacteria – some good and some bad, and it’s vital that you keep your mouth clean just as you would your hands and any other part of your body. You should aim to brush your teeth twice a day, and ideally with a soft to medium brush so that you don’t do damage to your gums and enamel.
Learn how to properly look after your mouth and teeth with this helpful list of suggestions to follow below:
Remember To Floss
By only brushing your teeth alone, you’re not cleaning the entire surface of any tooth. You should clean in between them in order to remove the hard-to-reach build-up of food and tartar. Over time, these pieces of food can begin to putrefy and create a foul odor. This should be enough to put you off, and run for the floss immediately!
You should aim to floss your teeth each day and do it carefully so as not to put excessive pressure on your gums and cause them to bleed. Flossing, and rinsing with a fluoride mouthwash will enable to you enjoy better overall mouth health, so what are you waiting for?
See The Dentist Without Delay
Many people don’t enjoy their bi-yearly trip to the dentist, and this is mostly because they’re worried about what they might learn. You should try to unlearn this, simply because not going can have some pretty serious consequences and impact your health.
If you haven’t attended a dental practice for a while, then register with your local dentist without delay and book the earliest appointment available to you. If you’re concerned or nervous, then find out as much as you can on what to expect from teeth cleaning at the dentist as well as fillings, for example. Doing this can put your mind at ease, and actually turn up to your appointment feeling calm rather than nervous.
Protect Your Teeth
There’s more to looking after your teeth than just cleaning them thoroughly. You should protect them from injury as well. If you play sports, then it’s vital that you wear a mouthguard to shield them from potentially damaging impact. Sports such as hockey, rugby, and martial arts require that you protect your teeth from start to finish, so never play these sports without wearing the proper gear. It’s just not worth the risk and losing your teeth as a result.
Mouth and tongue piercings can cause dental trauma, and you might be better off not having them. If you do, then try to remember to remove them before you eat and before you go to sleep as well. Further protect your teeth and gums by steering clear of sugary and fizzy drinks as they can weaken the tooth’s enamel and cause serious and unattractive damage, stains, and tooth loss.
Do It Yourself (DIY) has become all the rage, especially in healthcare. WebMD has become more trusted than the local physician. And soon, you’ll be able to go to a pharmacy and get all sorts of medical and dental help. Oops, that’s already the case!
As you may have heard, Smile Direct Club, which offers at-home clear tray tooth alignment services, will be coming to hundreds of CVS pharmacies around the country. Increased access? Yes. Safe? No.

At Linhart Dentistry, we have a Board Certified Orthodontist who performs Invisalign, all done under strict supervision.
Of course, Do It Yourself often means that if something doesn’t work, you’re going to have to Fix It Yourself (FIY) too. Often, that’s because you’ll feel embarrassed to bring the issue to a real doctor for fear of them chastising or mocking you for doing something so stupid.
So there’s another raging trend, FIY after you’ve tried DIY.
We realize that there’s an almost irresistible urge to do something that seems expedient, inexpensive and innocuous, such as simply moving your teeth into alignment.
However with most medical and dental DIY schemes, the consequences of not using a DIY solution properly or delaying proper treatment effects your most valuable possession, your health.
We’re like you and love saving money. And frankly, there are some areas where DIY can work. Taking meticulous care of your teeth and gums is a DIY system that dentistry has promoted for decades. Brushing, flossing, and other treatments prescribed by your dentist and hygienist are essential for health. And they work!
But saving money on your groceries is very different than skimping on your health.
So when you see a NYC Subway ad for at-home braces, or a billboard touting the next miracle weight loss cure, it may be a good idea to visit your healthcare provider before diving in. There are many reasons that these procedures have traditionally been prescribed and administered by licensed professionals.
The barber-dentist-surgeon, for better, is a thing of the past!
The take away here is; if you’re thinking about using a dental DIY product or scheme, ask us first. And, if you have used one and it hasn’t worked or worse, it made things worse, don’t try to FIY.
We’re here and happy to help you. And, we might even recommend a DIY solution if we think it’s appropriate.
– The Linhart Dentistry Team
The “Big Game” is behind us. And, for the most part, the game was dull and viewership was down. To most of us, the best part is watching the commercials! Especially this year.
The commercials tell us a lot about the US consumer and what is “hot” in America. After all, at $5.25 Million per 30 seconds, a lot of market research goes into these ads.
This year, it was interesting to see that along with the many alcoholic beverages, perennial regulars Coke and Pepsi, 2 other “sparkling” drinks entered the market; One soft (Bubly) and one hard (Bon And Viv Spiked Seltzer). People think that “SPARKLING” is healthy. In fact, Bubly’s tag line says “JUST SMILES”.
:max_bytes(200000):fill(white)/http://dcmzfk78s4reh.cloudfront.net/1520186327779.jpg)
And with dozens of new and hip sparkling drinks on the market, more and more of us are turning to them instead of good old tap water.
And, everyone it seems is anti sugar (and corn syrup). While that’s a good thing for our nationwide obesity epidemic, it doesn’t deal with another common phenomenon, TOOTH EROSION!
The problem is that we’re seeing an increasing amount of tooth sensitivity and “erosion”. Erosion is where the tooth is actually melting away, much like the Wicked Witch of The West in the Wizard of Oz, when water is spilled on her, teeth melt away when exposed to acid.
Sparkling anything means carbonation. And, carbonation means carbonic acid. And acid, well, as you can imaging, dissolves teeth. It dissolves the enamel and the softer dentin and root surfaces. The result is weaker and more sensitive teeth.
The average pH (the measure of acidity, with 7 being neutral, >7 being basic, and <7 being acidic) of carbonated drinks is 2.5-2.8, only slightly less acidic than battery acid!

Tooth enamel starts to dissolve at pH 5.5, you do the math! Dentin and root surfaces will start melting away at just pH 6.5.
And, when you add SUGAR to the acid, guess what also happens quicker? CAVITIES!
And, when you’re taking medications that dries out your mouth, guess what happens even faster? MORE CAVITIES!
And if you think its just carbonated drinks, think again. Here’s a list of some foods and their pH.
Beer 4.0-5.0
Black Tea 4.2
Cranberry Juice: 2.5
Cranberry Sauce 2.3
Coffee 2.4-3.3
Fermented Veggies 3.9-5.1
Orange Juice 3.7
Ketchup 3.7
Pickles 2.5-3.0
Carbonated Drinks 2.5-2.8
Tomatoes 3.7-4.7
Sodas, like Coke and Pepsi are pH 2.4. And, the diet versions are NO BETTER!
These are EXTERNAL sources of acid too. If you have indigestion, pregnancy nausea or GERD (acid reflux) your stomach acid (pH 1.5-3.5) might be adding to the problem.
What are you to do???
- Minimize exposure: try NOT to sip your acidic beverage over a long time. The sooner it’s gone, the better.
- Eat Fibrous foods. Foods that have fiber and require a lot of chewing stimulate more saliva, which neutralizes (buffers) the acids. Saliva is BASIC.
- After eating anything acidic, rinse your mouth with water. Don’t swish anything bubbly around! Tap water in NYC and the area has fluoride, which helps strengthen Enamel.
- Don’t brush within 30 minutes of eating anything acidic (almost anything). That just allows the bristles to work the acid into the tooth material faster, accelerating the erosion. Also, NEVER SCRUB with a toothbrush, your teeth are NOT the dishes!
- Drinking acidic beverages through a straw helps protect teeth a bit, but not back teeth.
- Chew sugarless gum with either Xylitol or Erithritol. These natural alcohol sugars are safer and actually change the bacteria makeup of the mouth. Chewing, as I mentioned above, stimulates saliva, your body’s natural defense system. Please check with us to see if chewing gum could harm your joint (TMJ) or your dental restorations.
- Fluoride helps make the teeth (especially the roots) more resistant to acids. Please ask your hygienist which form of fluoride is most appropriate for YOU.
- LINHART toothpaste has Xylitol, and Fluoride, to help keep enamel strong. Also, Theobromine, an extract of chocolate, is included to strengthen enamel.
We try to customize our dental recommendations based on your specific risks. Along with educating you, it’s how we can best help you prevent problems.
Modern dental practice is so comfortable and pleasant that almost all patients can tolerate or even enjoy their time in the dental chair. Effective and gentle local anesthesia with or without the use of nitrous oxide (laughing gas) allows nearly everyone to experience dental work with minimal stress. A light oral sedative can be given to a patient prior to dental treatment and is an option that helps allay anxiety, and promotes a relaxed yet awake state of consciousness.
At Linhart Dentistry, we are able to perform the most simple cleanings, to complex procudures like Porcelain Veneers, Dental Implants, and Full Mouth Rehabilitation under all different forms of anesthesia.
Some patients can benefit from or even require deeper sedation during their dental procedures than nitrous oxide, lidocaine (novocaine), or numbing gel.
Patients with extreme anxiety about dentistry may not be able to tolerate being awake at all during any but the most minor dental procedures. These patients may have suffered traumatic dental experiences as children or may have had difficulty “getting numb,” or even may have an intense gag reflex. Dental anxiety has prevented many patients from getting dental care for years (even decades!), resulting in a cycle of untreated dental decay, increased sensitivity and dental pain, and increased fear. Once a patient’s dental health has been restored (which may require several sessions under sedation), the patient now has healthy teeth, pain is eliminated, and often the dental phobia has lessened as well, allowing the patient to follow up with routine dental care while awake.
Many individuals with Special Needs such as Autism may not be able to tolerate any dental work at all while they are awake. Children who require extensive dental restoration may also not be able to cooperate for longer procedures. Often these patients are referred to a hospital setting for care, but Sedation Dentistry in the office may be a safe, less stressful and more pleasant option for many of these special patients and their families. At times a premedication may be given to help these patients tolerate intravenous placement (an IV), and then a rapidly acting, rapidly eliminated sedative is given to allow the patient to undergo a variety of dental procedures, including x-rays, cleanings and restorations. For many patients, Sedation Dentistry allows for the completion of necessary dental care that otherwise would be impossible.
Sedation Dentistry has been safely administered to thousands of patients in an in-office setting. The highest standard of care is by a Board Certified Anesthesiologist with vast experience in Office-Based Anesthesia, and Anesthesia for Dentistry in particular. Safe sedation begins by having patients complete a pre-anesthesia questionnaire and an evaluation by their private medical doctor. The anesthesiologist will review this information and then speak with the patient well in advance of the procedure to formulate the optimal sedation plan. During Sedation Dentistry the anesthesiologist continuously monitors the patients’ vital signs and administers just the right amounts and combinations of medication to achieve safe and effective sedation. Patients sleep safely throughout their dental work and awaken with the good news that the procedure has been completed!
Dr. Nadine Keegan is a board certified Anesthesiologist and has worked for years with Linhart Dentistry to provide comfortable treatment to our patients.
Please contact us if you have interest in anesthesia and sedation for your next visit!
– Nadine J. Keegan MD


Also known as DIY, it has become a hot subject in the health field. After all, with healthcare costs rising, increased waiting times for Doctors and a generalized disgust with the entire system, the urge to just “do it yourself” can be enticing. However, DIY medicine comes with a slew of risks and dangers that you may want to avoid at all costs!
There are plenty of companies willing to take your money and help you out.
Do it yourself anti-depression treatment, hair regrowth, anti-snoring, arthritis remedies, headache relief, teeth whitening, and even teeth straightening systems are available.
Do it yourself therapies pander to our society’s urge for immediate gratification and cost savings. Why go to a Doctor when you can do a search on the internet and get the DIY product delivered to your door in a day, and for ½ the cost?
Yet, we know that immediate gratification can come at a cost that time not money can account for. Often, this cost is not realized until years down the road.
It’s estimated that up to 20% of people who use DIY products can actually be harmed by them. Part of that computation takes into consideration the fact that people who diagnose themselves incorrectly and use a DIY product, might be deferring effective treatments and could lead to significant worsening of the underlying disease.
And where’s the FDA and protection from the government?
Take the anti-snoring product, which rhymes with Zipper and is being heavily promoted by a Soprano’s sounding character all over the radio. While this product might, in fact, reduce or even eliminate snoring in some people, it can actually mask underlying, life-threatening problems such as Obstructive Sleep Apnea (OSA) or Central Sleep Apnea (CSA).
It’s estimated that 50% of people who snore have some significant underlying and perhaps even life threatening problem, such as Sleep Apnea. And yes, Sleep Apnea can lead to DEATH. And an at-home appliance may mask the symptoms associated with Sleep Apnea.
And what about the significant potential for TMJ problems and teeth shifting that are common with any improperly fitted and monitored DIY mouth device?
You see, snoring is a symptom. And, most DIY products are aimed at relieving a symptom, not the underlying issue.
What you should always ask, as we at Linhart Dentistry do, is: What’s causing the symptom? It sounds logical; find out what’s causing the symptom and treat the underlying cause first. Then, the symptom will disappear. Sounds like common sense!
But, as the great Benjamin Franklin said; “common sense is very UNcommon!”
Our healthcare system is guilty of treating symptoms rather than discovering and resolving causes. It’s the basis behind all the pop-up clinics and “Doc-in-the-box” Emergency clinics so ubiquitous today.
Linhart Dentistry is bucking this trend. We believe that uncovering causes, while perhaps taking more time and even costing a bit more up front, yields more predictable, sustainable and less costly care in the long run. We believe that health is a marathon, not a sprint.
So why aren’t others following Linhart Dentistry’s lead? The answer to most of these questions is; Follow The Money!
There’s more money in treatment than there is in thinking and diagnosing causes. Thinking and diagnosing takes time! It’s just a matter of economics.
But we’ve always believed in the philosophy of ‘putting your money where your mouth is’. We think our investment in technologies and taking the time to help diagnose underlying causes is well worth the effort…in the long run…FOR YOU.
So the next time you see an at-home treatment for snoring, teeth-straightening with invisible aligners, whitening, or arthritis, ask your qualified health care professional what the RIGHT treatment is for you!
Medical Perils of the Internet
There’s a new disease out there to be wary of. “Cyberchondria” is caught by surfing the web for medical information.
Would you accept medical advice from a stranger on the street? That’s what most of the Internet consists of; a bunch of strangers. The Internet can indeed be a tangled, impossible to navigate, web when searching for medical information.
You might think that you can search published medical (or dental) journals and get accurate information but that’s not necessarily the best strategy. Journals often publish obscure and challenging cases that probably won’t give you information about what you’re looking for. Even seasoned professionals often have a difficult time sifting through these articles to extract the relevant information.
A recent scientific article looked at the search habits of people before they showed up to the Emergency Room. What they found was that 80% of the people who looked things up online reported that their searches actually improved their subsequent ER experience. They felt that they were better able to communicate symptoms and understand what the Doctor was telling them. So, the conclusion was that looking things up can be helpful.
But “search” has challenges too. A search for “endometriosis”, the subject of over 4.5 million searches a year, showed that only ONE of the top 54 results contained accurate information. That’s scary. The best sources of information are from trusted sites such as Academic Institutions, Medical Centers or other professionally monitored sources whose information is vetted. Going to Pubmed or Google Scholar might not be as fruitful as going to The Mayo Clinic, Cleveland Clinic or Harvard Health.
And of course, one wouldn’t want to spend 20 minutes searching for the symptoms of a stroke, if that’s what’s happening, when you could have called 911 first!
In dentistry, the problem of search is just as perplexing. There’s a lot of bad and wrong information out there. That’s why we’ve begun sending out these email-newsletter-blogs. We want to be your trusted source of information.
We believe that the best medicine (and dentistry) is personalized. The Internet, at best, presents “One size fits all” solutions. At its worst, it presents “worst case” scenarios. Most problems are often in between. It’s “off the rack” advice. We prefer custom, individualized solutions and advice.
So here’s an invitation. If you have a symptom, problem or question, go ahead, do some Internet searching. Then, either call or email us. We’ll gladly answer your questions or give you advice based on what we know about you as an individual.
We’re here to help you at Linhart Dentistry. And, with our team of highly experienced specialists, we can give you the most accurate and best information possible. Whether its gums, teeth, tongue, TMJ, whitening, Invisalign, Sleep or snoring appliances, Cosmetics, Implants or any dental “search” you can think of, Linhart Dentistry has your answer. Just ask!

Gum recession is a dental condition that’s caused by the withdrawal of bone supporting gum tissue. This leads to irritation because it exposes the roots of the teeth.
The root is the lower 2/3 part of your tooth that’s not visible but it houses the blood and nerve supply of that region.
You won’t experience receding gums if your jaw bones are intact to hold everything in place.
So what causes receding gums? Look at some of them.
Causes Of Gum Recession
1. Overbrushing
Aggressive brushing. Rough brushing. Or overbrushing if you like. They’re all talking about the same thing. Your failing to develop an appropriate dental technique because you believe that pressure has something to do with a white smile.
Can you replace a toothpick with a needle to get little food particles off your tooth? You’d hurt yourself, right? That’s exactly what happens when you brush roughly. You injure your gums, causing bleeding gums and initiating gum recession in the process.
Aggressive flossing is also a factor.
2. Whitening Strips
And all other whitening formulas you’ve ever heard of. If you’re using them after consultations with your local dentist then that’s not a problem.
Problems usually arise when there’s an excessive use of these chemicals as they contain very corrosive ingredients that can destroy the gums.
3. Gum Disease
And a very common one is gingivitis, the inflammation of the gums. Gingivitis makes the gum swell, causing bad breath and degenerating into periodontitis if it’s not checked.
Gum recession is one of the symptoms too. And that’s because the inflammation in gum disease causes deterioration of the jaw bone.So check with the dentist if yours is a sign of a deeper infection.
4. Bruxism
So you had a rough day at work. Do you ease off by clenching and grinding your teeth at night? Maybe that’s what’s causing your receding gums. Grinding teeth weakens the structure of your jawbones.
5. Trauma
I’m sure you know what can happen to your canines if you’re constantly smacking them on every wall you find. They could get chipped or even fall off completely. So a traumatic injury to your teeth can cause receding gums.
6. Genetics
This post has been all about how your jaw bones support your teeth and why that strength is needed to prevent gum recession.
But what if it’s not all in your control. Every physical feature you’re endowed with has a thing or two to do with inheritance. The thickness or thinness of your jaw bones too.
Though very uncommon, genetic disorders like Marfan Syndrome and Parry Romberg Syndrome cause thinning and underdevelopment of the jaw bones.
And if your teeth are abnormally positioned, gum recession could set in also.
7. Poor Oral Hygiene
Think of every dental infection that could be caused by poor oral hygiene. I’m talking things like a dental abscess and periodontitis. These infections have gum recession as symptoms and that’s why poor hygiene is a factor you can’t ignore.
So you don’t confuse gum recession with any other dental infection, here are some signs you should look out for.
1. Longer Teeth
If you suspect anything, just compare the present length with maybe an old photo, or ask a roommate to check.
2. Exposed Root
Gum recession exposes the root section of your teeth, so you’d see different colors when you look in the mirror. The white or greyish look of your crown would be followed by a brown section underneath.
That’s the root that has been exposed.
3. Loosened Teeth
The jaw bones can no longer support the teeth so the teeth are severely weakened, even shaking at times.
4. Irritation
The exposed root exposes the blood vessels and nerves so you’d begin to feel sensitive to hot, cold and acidic foods. Pain signals are also transmitted.
5. Inflamed and Bleeding Gums
The margins of your gum would show patches of swelling that bleed when you brush or eat foods that need you to do a lot of chewing.
So how do you stop this?
5 Ways To Stop Receding Gums
1. Avoid Overbrushing
Pressure is not proportional to the brightness of your teeth. So focus on applying the right amount of pressure.
If that’s something too hard for you, get a toothbrush with a pressure sensor so you don’t injure your gums.
And you should consider getting a toothbrush with soft-bristles, it still gets the job done and is gentle on your teeth and gums.
Follow standard practice too. The ADA recommended brush-time is two minutes, don’t try to brush for five minutes. And you should brush twice daily also.
2. Adopt Proper Oral Hygiene Techniques
Flossing, rinsing, reducing sugary-food intake are practices that can prevent some of the consequences of poor oral hygiene.
3. Seek Help
If you’ve been involved in any traumatic attack to your teeth, see a dentist to examine the extent of damage. Check if you’d be needing any dental crowns or bridges if you have a chipped tooth.
And wear protective gear if you’re involved in contact sports or hunting.
If there’s any formula or whitening technique you want to try, consult with your dentist first so you don’t try something that’d erode your enamel.
4. Get A Mouth Guard
A mouth guard reduces the impact clenching and grinding have on your teeth so ask your dentist if this is something he’d recommend.
5. And All The Home Remedies
The anti-inflammatory properties of green tea check gum inflammation and strengthen the attachment of gums to the teeth.
Aloe Vera can reduce gum texture by restoring the right texture of gum tissue.
Coconut oil has antimicrobial agents that fight inflammation and reduce gum recession.
Lemon oil is antiseptic. It attacks the bacteria that act as causative agents to kick-start inflammation. It also has a pleasant smell that fights bad breath caused by bleeding gums.
A deficiency in vitamin C can cause bleeding gums so you should ensure you don’t have low vitamin C levels at any time.
Receding gums aren’t something you should take lightly. They’re dangerous on their own and could also appear as signs of other infections.
But now you know the signs to look out for, the causes and how you can stop this anomaly.
Dr. Levi Spear Parmly, a New Orleans dentist, invented floss in 1815. Flossing has been touted by dentists since as being the most effective way of preventing cavities and gum disease. Is it true?
Flossing is something most people think they need to do. After all, every dentist and hygienist I’ve ever met thinks flossing is imperative for good oral health. Yet, according to statistics, only 12% of Americans floss daily and 49% don’t floss at all.
The controversy about flossing was fueled by a NY Times article several years ago that discussed the matter and the fact that the US Department of Agriculture and the Department of Health and Human Services dropped the mention of flossing as part of their hygiene recommendations due to lack of “evidence based” studies.
So what’s the scoop? Should YOU floss or not?
YES, you should, but it’s not always so simple. Unfortunately, as in most healthcare matters, there’s no simple answer as to whether flossing is righ t or wrong, effective or not? It’s complex and based on your personal, unique and individual needs and risks.
t or wrong, effective or not? It’s complex and based on your personal, unique and individual needs and risks.
Every time you visit our hygienists, they evaluate the “effectiveness” of what you’ve been doing vis a vis your oral health. They ask about your medical health and any changes because we know how that can impact your mouth. They look for cavities, gum inflammation, tongue health and even cancer. They scrutinize all aspects of your mouth to make sure all is well. And, if there are areas of concern, they bring it to the attention of your dentist.
We want to help your mouth stay healthy because we know it will contribute to your overall health and wellness.
So, we might recommend that you change what you’re doing. We might recommend that you floss. We might recommend that you don’t and use some other method to clean between your teeth, like inter-dental brushes or an air flosser.
We might also recommend that you take a bacteria profile so we can see what’s happening microscopically. We might recommend that you use a different toothpaste, rinse or even an oral probiotic. We might recommend that you come to see us more frequently.
Indeed, in some cases, there are more effective systems than flossing to clean the “between the teeth” areas that can help prevent gum disease and especially, root cavities.
Your visits to the hygienists in our practice are often the most important for long term oral health. And for those who have invested a lot of time effort and money into their mouths, these maintenance visits pay off handsomely. They are indeed, the best return on investment you can make.
So floss, but we also may recommend adjunct treatments to help you clean between your teeth.
So, we’ll see you soon at your visit with one of our fantastic hygienists!
– The Linhart Dentistry Team
That’s the sound Rice Krispies are supposed to make when milk is poured over the popular breakfast cereal. It’s NOT what’s supposed to happen when your mouth opens or closes.

Creaky, crackling and noisy joints are symptoms that might be predictive of problems that could, if not dealt with, result in limitations of jaw movement such as lock-jaw. Imagine not being able to open your mouth wide enough to eat a sandwich? Or, what about not being able to chew without pain?
Some people haven’t been able to eat a Subway sandwich without pounding it down, all their lives. They just think such limitation is normal. If you can’t get at least 3 finger widths between your teeth, you might have a TMJ issue.
The jaw joint or TMJ, temporomandibular joint, is unique in the body. It’s a double joint, with one bone, the lower jaw suspended via a joint at either end. Movement of the lower jaw position is controlled by these joints and by the muscles, tendons and ligaments that attach to the head, jaws and neck.
Most often, joint sounds are innocuous. Many people don’t know they have any. Your dentist should include an examination of your TMJ’s as part of a comprehensive examination.
Sometimes, joint sounds are problematic. They can be indicative of a misalignment in the joint, arthritis or inflammation. In a car, such a misalignment will cause the tires to wear out unevenly. The same thing happens in the mouth, as teeth can also wear out.
How does a misalignment of the jaws happen?
The usual reasons are; wear and tear, clenching/grinding, muscle imbalances, sleep position, sleep disturbances, trauma, poor posture, stress, mineral deficiencies/overload and even medications.
Medications? Every drug has some unintended consequence. Some of the more common ones that can affect muscles are:
➢ Diuretics (like Lasix and hydrochlorthiazide),
➢ Procardia (for angina and hepertension)
➢ Proventil, Ventolin, Brethine (for asthma)
➢ Statins like Lipitor and Crestor(for cholesterol)
➢ Evista (used for osteoporosis)
➢ Antidepressants (Paxil, Zoloft, Prozac, Celexa, Lexapro and other SSRI’s which can also be used to treat ADHD)
Millions of Americans take one or more of these medications. Yet, most people and even most doctors don’t associate the symptoms of muscle issues with these medications. The most common muscle complaints involve painful leg cramps, which might never be associated with medication use. But, such cramps and spasms can happen in any muscle.
Another common symptom of “TMJ” is fullness or even ringing in the ear (called tinnitus). These too can be signs of muscle issues. And to prove it to yourself, clench your teeth together tightly. When you do, does the background noise change a little? That’s because the muscles that close the jaw also have an affect on the ear.
Treatment of “TMJ” involves first making the proper diagnosis. Then appropriate recommendations for treatment can be made, which might include, self-care, medication modification, bite guards, physical therapy, orthodontics, bite adjustments and sleep appliances.
The takeaways here are:
- Pay attention to joint sounds or changes
- Bring such changes to your dentist or hygienist’s attention
- Tell your dentist and hygienist about all the medications you take
Your TMJ’s are too important to take for granted.
Article by:
Dr. Michael Goldberg and the Linhart Dentistry Team
